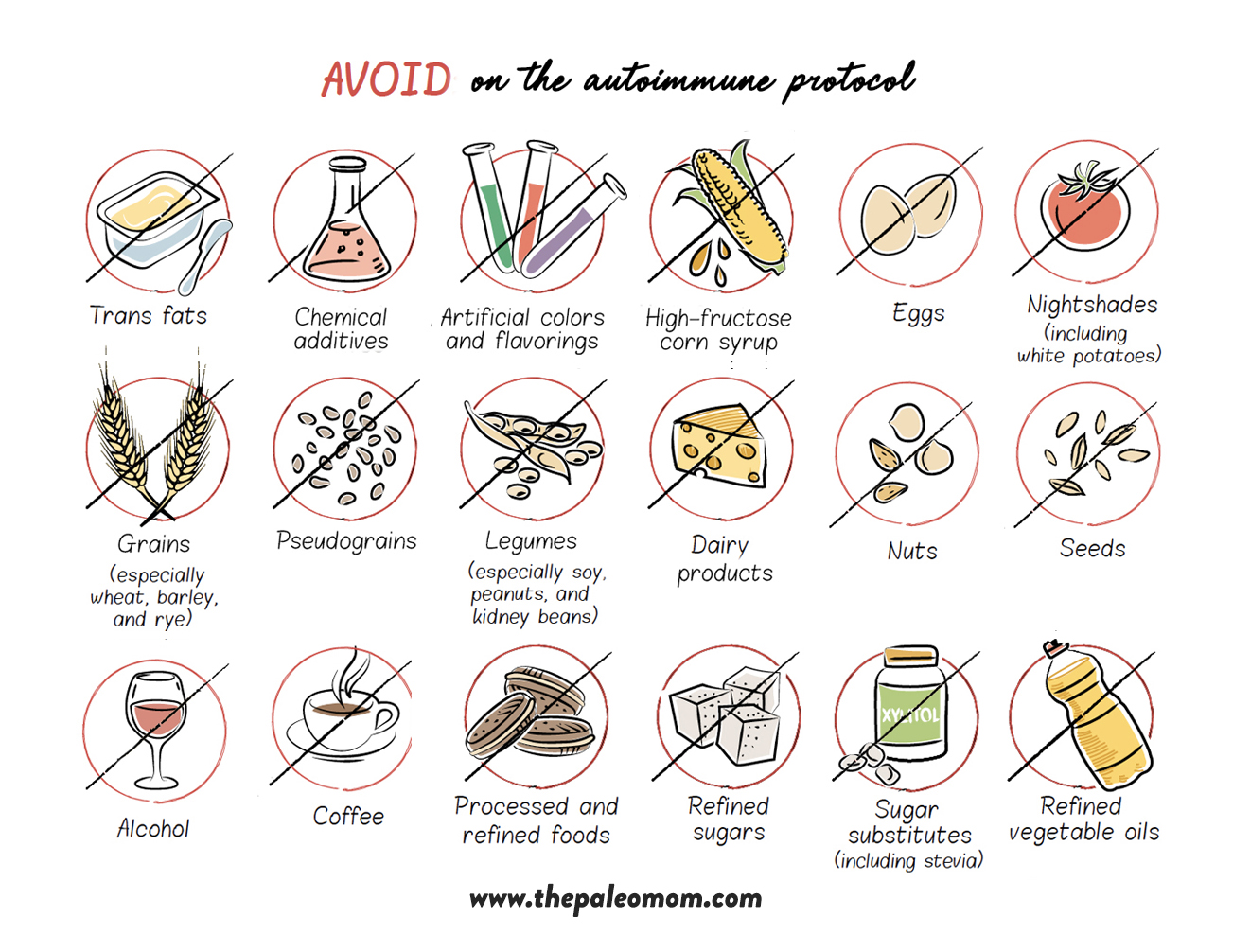
The Autoimmune Protocol can be thought of as a nutritional intervention for a diet gone badly awry, overabundant in calories and lacking in vital nutrients. But how well an individual tolerates suboptimal foods—whether we’re talking about something like tomatoes, which are included in the Paleo diet but eliminated on the Autoimmune Protocol, or something like grains, which are not included in either nutritional approach—depends on nutrient status, stress, sleep, activity level, genetics, and health history. As we improve these factors with diet and lifestyle changes, it’s fairly common to see tolerance of certain foods increase.
It’s important to emphasize that the AIP dietary framework is not a one-size-fits-all diet that autoimmune disease sufferers are doomed to follow for their entire lives.
In fact, the AIP can more accurately be described as a sophisticated elimination and challenge diet that embraces self-discovery via its Reintroduction Phase and respects bioindividuality via its Maintenance Phase (see also The 3 Phases of the Autoimmune Protocol). In this regard, the AIP is more like a step-by-step plan to help you identify your autoimmune disease triggers, truly understand the diet and lifestyle requirements of your own body, and hone in on a personalized plan that works for you as an individual and is sustainable for your entire life. You can think of the Autoimmune Protocol as encompassing three phases: Elimination, Reintroduction and Maintenance.
The Reintroduction Phase of the AIP is your opportunity to truly understand your body’s needs, identify your trigger foods, and hone in on your personalized optimal diet for lifelong health. Many people also test the boundaries of lifestyle factors during the Reintroduction Phase, further identifying what lifestyle priorities are most important to maintain their health and what they can let slide from time to time. You might also discuss with your healthcare provider the merits of discontinuing specific medications or supplements in this phase, if you feel that they might no longer be needed.
Elimination, Challenge and Immune Tolerance
Identifying a link between specific foods and how we feel can be tough when we’re chronically exposed to those foods, for a variety of reasons:
- We adjust to how bad we feel, making it difficult to realize that we don’t feel our best.
- Our bodies can upregulate protective mechanisms, like producing more mucus in the gut, that can restrain reactions to a degree that makes them difficult to recognize.
- Symptoms can be amorphous—like feeling fatigued or moody—and we may not experience them immediately following consumption.
 Elimination diets, like the AIP, work by removing all these limitations.
Elimination diets, like the AIP, work by removing all these limitations.
Cutting out the foods that we may be reacting negatively to gives our bodies time to detoxify and recover from any negative health impacts. Many people express feeling renewed energy and well-being after adopting a Paleo or AIP diet, typically within a couple of weeks. When you’re feeling great, it’s easier to identify that you don’t feel your best when a challenged food causes symptoms, even if those symptoms are fairly mild. The elimination phase also allows for the downregulation of any protective mechanisms, which means that reactions can be exaggerated and obvious when we consume foods that don’t work for us. Finally, a methodical challenge protocol allows us to identify problematic foods even when our symptoms are vague and occur days after consuming those foods.
Let’s take a moment to discuss exaggerated reactions to eliminated foods upon challenge. Exaggerated reactions typically occur in the case of food allergies and intolerances, and they can be very frustrating. It’s common for people to misinterpret exaggerated reactions as AIP (or Paleo) “making them intolerant” to foods such as wheat. But that’s not the case; in fact, the mechanisms behind these exaggerated reactions are exactly why elimination and challenge diets are the gold standard for identifying food sensitivities.
Even in a perfectly healthy gut, food-protein antigens are absorbed by a number of different cells, processed, and then presented to the immune system via a process called antigen presentation as part of the body’s constant patrol for infectious agents. A type of sentinel immune cell in the gut called dendritic cells stick a long, armlike protrusion, called a dendrite, between enterocytes and into the lumen (inside) of the gut to “sample” the gut environment in search of infection. They then migrate to the gut-associated lymphoid tissues to present the antigens they’ve found (antigens from invading pathogens or food antigens) to other immune cells (naïve T cells and B cells). Other cells can do this same job, including a type of cell called an M cell in the Peyer’s patches and even enterocytes themselves. It’s a little like sticking your toe into a lake to see how cold the water is before you decide whether or not to jump in—the immune system is constantly grabbing food proteins from the gut and showing them to our immune systems so our immune systems can decide whether or not to react. (See also What Is the Gut Microbiome? And Why Should We Care About It? and What Is A Leaky Gut? (And How Can It Cause So Many Health Issues?))
That’s right: our immune systems don’t react to all antigens all the time. It can “choose” not to react to an antigen through a process called immune tolerance.
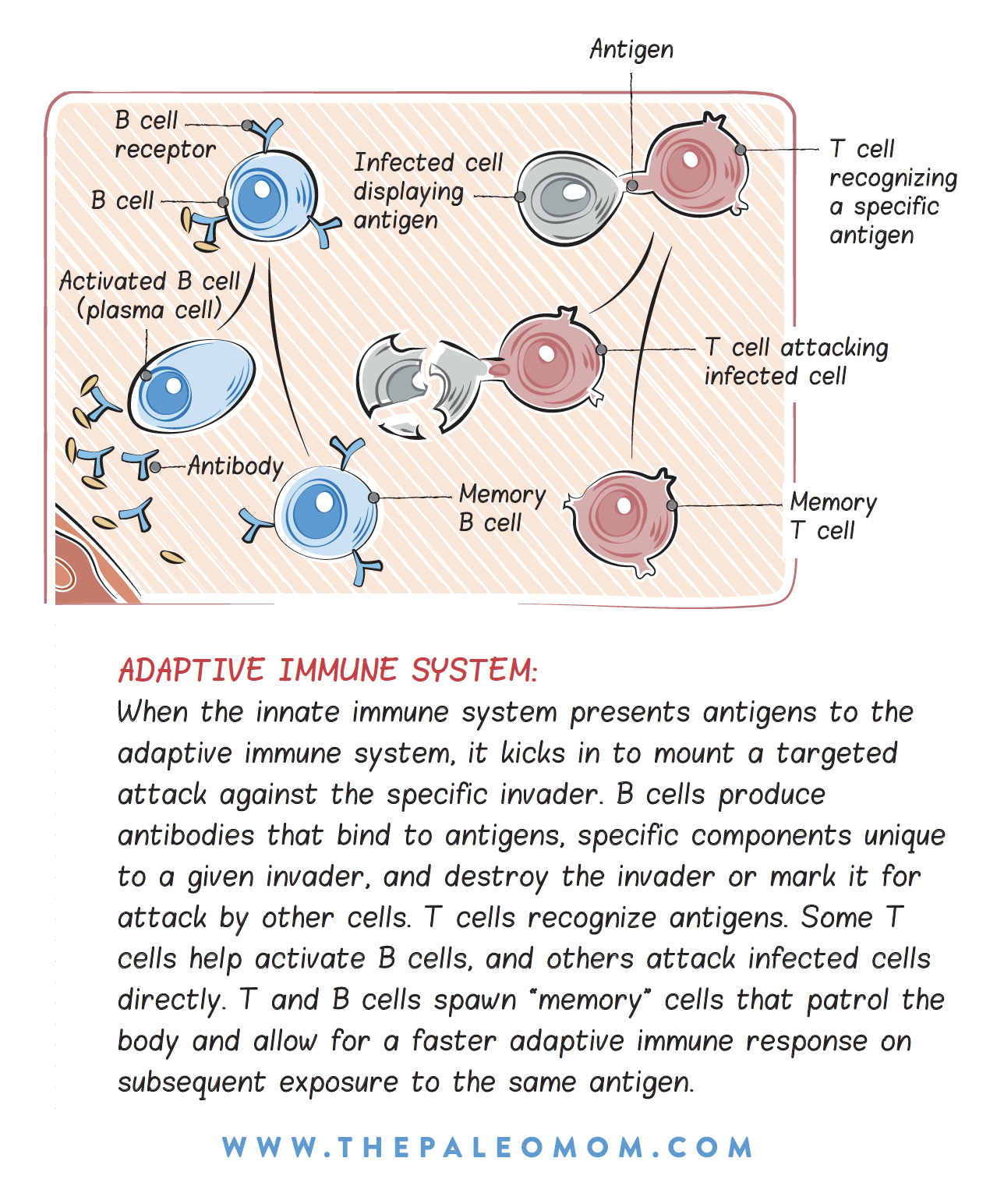
Immune tolerance is mediated by regulatory cells of the adaptive immune system, called regulatory T cells. These cells can suppress the activity of those cells propelling an immune response to a food antigen (Th1, Th2, and memory cells) by producing anti-inflammatory cytokines (chemical messengers) that inhibit immune-cell activation, or they can actually cut the receptors off of immune cells so that they can’t bind to the food antigen. But here’s the kicker: these regulatory cells tend to have a shorter lifespan than the immune cells (there may be a genetic factor at play here since the lifespan of these cells can vary from a few days to months). If you have an immune reaction to a specific food, there is the period after eliminating it when the immune cells responsible for the reaction are still hanging around but the regulatory cells responsible for immune tolerance are too low in number to constrain the reaction. This is called loss of immune tolerance, and it is one cause of the exaggerated response to a challenged food. See also Can Paleo or AIP Diets Cause Loss of Immune Tolerance? and Development of Immune Intolerance in Children
Immune tolerance is generally considered to be a good thing, but, of course, if you don’t have an immune reaction to a food, you don’t need to develop immune tolerance to it. The more a protein is broken down by healthy digestion (and compatibility with our digestive enzymes), the less immunogenic (immune-stimulating) it is when it’s “sampled.” In fact, the mere act of restoring healthy digestion can make many food sensitivities disappear. Immune tolerance also relies on how much of an antigen crosses the gut barrier because memory cells tend to reside over the long term in the spleen. In the case of a leaky gut, much more of a specific food antigen can cross into the body than when the gut barrier is intact, getting into the circulation where the food antigen can activate memory cells in the spleen, stimulating an immune response. Once you have a healthy gut barrier, the “sampling” of antigens becomes a much more tightly controlled process, and antigen is unlikely to get into the circulation.
 Other factors may be at play in an exaggerated response to a food upon challenge. Perhaps the mucus layer of the gut was thickened as a protective mechanism before you eliminated the problematic food—basically, your body’s way of minimizing your exposure to an antigen. Now that your body is healing, the mucus layer is thinner, so when you do eat a food to which you are allergic or have developed an intolerance, more of it can interact with your immune system. For most people, these dramatic reactions will diminish over time, especially as gut barrier and immune health improve. Eventually, the number of immune cells responsible for the reaction decreases as well, so even if a food cannot be successfully reintroduced into your diet initially, it’s worth trying again in a few months. In fact, a lack of serious reactions to foods is an excellent indicator of gut and immune health. By also addressing lifestyle factors (see The Paleo Lifestyle), you improve the chances of successfully reintroducing eliminated foods into your diet.
Other factors may be at play in an exaggerated response to a food upon challenge. Perhaps the mucus layer of the gut was thickened as a protective mechanism before you eliminated the problematic food—basically, your body’s way of minimizing your exposure to an antigen. Now that your body is healing, the mucus layer is thinner, so when you do eat a food to which you are allergic or have developed an intolerance, more of it can interact with your immune system. For most people, these dramatic reactions will diminish over time, especially as gut barrier and immune health improve. Eventually, the number of immune cells responsible for the reaction decreases as well, so even if a food cannot be successfully reintroduced into your diet initially, it’s worth trying again in a few months. In fact, a lack of serious reactions to foods is an excellent indicator of gut and immune health. By also addressing lifestyle factors (see The Paleo Lifestyle), you improve the chances of successfully reintroducing eliminated foods into your diet.
When to Reintroduce Foods
There are no hard and firm guidelines on when to reintroduce foods on the Autoimmune Protocol. I’ve always been hesitant to put a firm time frame on when to try reintroductions, because there seems to be a fairly large variability in how quickly people experience symptom improvement when they first adopt the Autoimmune Protocol (likely related to disease activity, genetic risk factors, nutrient deficiencies, digestion efficiency, underlying challenges, and specific implementation of the AIP diet and lifestyle).
As long as you’re seeing improvements in your health thanks to your diet and lifestyle changes, you can try some reintroductions after three to four weeks. If you aren’t seeing improvements after following the Elimination Phase of the AIP for 3 to 4 months, consider working with an AIP Certified Coach or functional medicine doctor to troubleshoot, rather than continuing to bang your head against the proverbial wall. (I also encourage you to examine the AIP Do’s and Don’ts to make sure you aren’t missing a fundamental piece of the protocol.)
Methodical is the name of the game. In general, reintroduce only one food every five to seven days, and spend that time monitoring yourself for symptoms of a reaction. It’s best to keep a food and symptom journal during this process too… the reaction to some foods builds over time and it can be difficult to identify the culprit without this record to review.
Don’t reintroduce a new food if you have an infection, have just had an unusually strenuous workout, got less sleep than normal, are feeling unusually stressed, or are under any other circumstances that may make interpreting a reaction difficult. If you have a hard time determining which food caused what reaction, wait longer between reintroductions. Even if a reintroduction is successful, you may wish to keep your consumption of the food to a minimum (like reserving a glass of wine for Sunday dinner) for the best long-term results. The foods you tolerate may change over time, too, so a failed reintroduction does not mean you can never eat that food again. It’s best to wait at least six months before revisiting a failed reintroduction.
Some foods that you reintroduce will also be relegated to “sometimes foods.” These will include alcohol and potentially some of the stage 4 reintroductions, like gluten-free grains. A sometimes food is one that doesn’t cause a reaction when you consume it occasionally, but that can subtly undermine your health (even if simply by displacing more nutrient-dense options) if you consume it on a regular basis. These are still worth reintroducing, even if they aren’t going to make it into your normal rotation, because they give you more flexibility in situations like travel and eating out. A thorough understanding of why each food is eliminated on the AIP is helpful for determining sometimes foods versus everyday foods, see AIP Eliminations Summary.
Reintroduction Procedure
The standard procedure for food challenge is as follows:
- Select a food to challenge. Be prepared to eat it two or three times in 1 day, then avoid it completely for a few days.
- The first time you eat the food, eat half a teaspoon or even less (one teensy little nibble). Wait fifteen minutes.
- If you experience any symptoms, don’t eat any more. If you don’t, eat one teaspoon of the food (a small bite). Wait fifteen minutes.
- If you experience any symptoms, don’t eat any more. If you don’t, eat one and a half teaspoons of the food (a slightly bigger bite).
- That’s it for now. Wait two to three hours and monitor yourself for symptoms.
- If you still haven’t experienced any symptoms, eat a normal-sized portion of the food—either by itself or as part of a meal.
- Do not eat that food again for 5 to 7 days, and don’t reintroduce any other foods during that time. Monitor yourself for symptoms.
- If you have no symptoms during the challenge day or at any time in the next 5 to 7 days, you may reincorporate this food into your diet.
It’s best not to be in a hurry to challenge foods. Generally, the longer you wait, the more likely you are to be successful (thanks to improved gut and immune health). But when you reintroduce particular foods is ultimately your choice. How you feel is the best gauge, and only you will know whether you are ready. A word of caution, though: don’t let cravings influence you. Your decision should be based on how good you feel and how much improvement you’re seeing in your health.
And on the flip side, don’t let fear of a reaction deter you. The goal of this self-discovery phase of the AIP is to truly understand your own body, the lines you can’t cross and your wiggle room, while expanding your diet! While a successful reintroduction is fantastic, even a failed one gives you valuable knowledge to help you navigate future situations!
Symptoms to Watch For
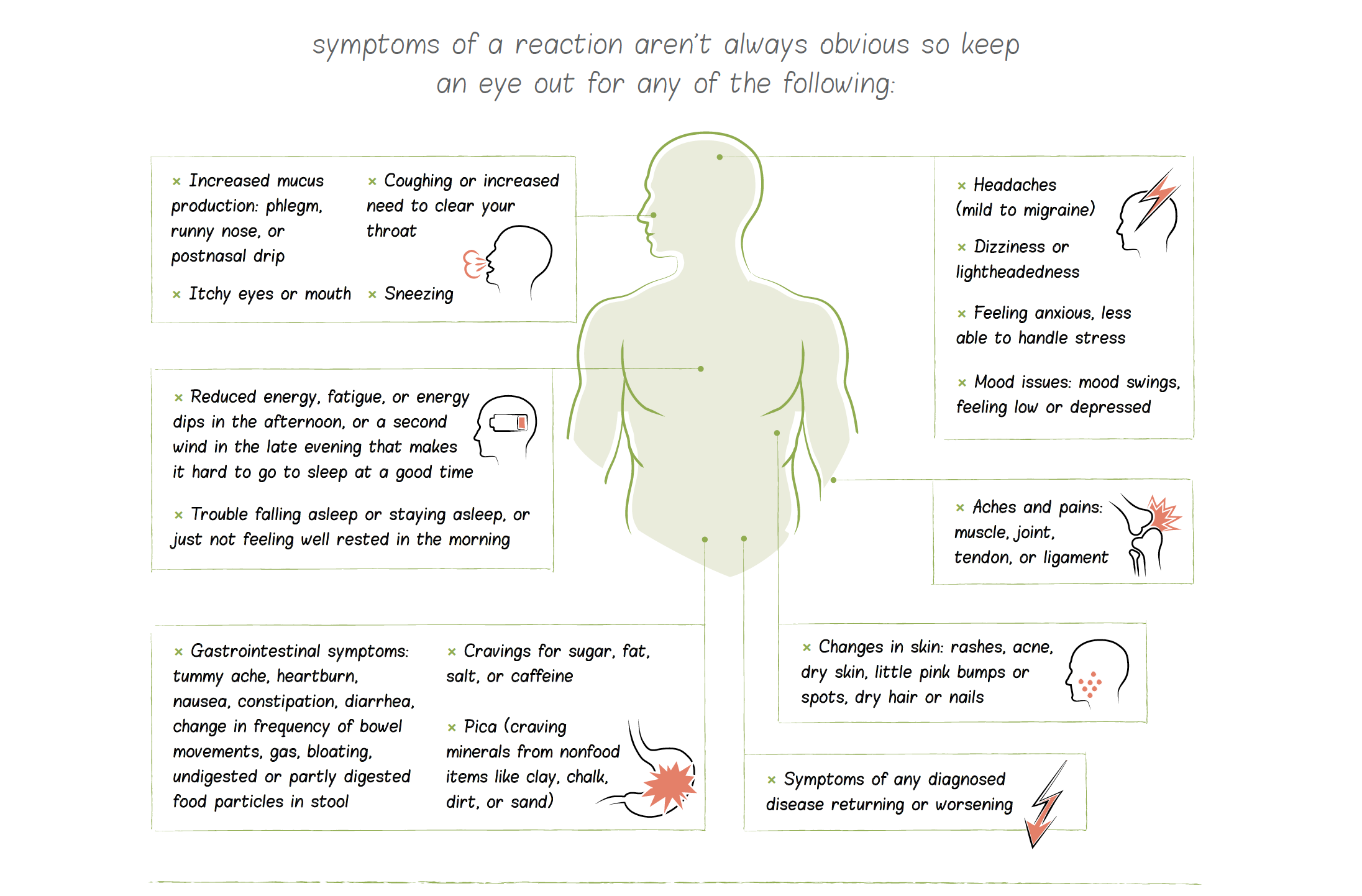
Symptoms of a reaction aren’t always obvious, so keep an eye out for any the following:
- Symptoms of any diagnosed disease returning or worsening
- Gastrointestinal symptoms: tummy ache, heartburn, nausea, constipation, diarrhea, change in frequency of bowel movements, gas, bloating, undigested or partly digested food particles in stool
- Reduced energy, fatigue, or energy dips in the afternoon, or a second wind in the late evening that makes it hard to go to sleep at a good time
- Cravings for sugar, fat, salt, or caffeine
- Pica (craving minerals from nonfood items like clay, chalk, dirt, or sand)
- Trouble falling asleep or staying asleep, or just not feeling well rested in the morning
- Headaches (mild to migraine)
- Dizziness or lightheadedness
- Increased mucus production: phlegm, runny nose, or postnasal drip
- Coughing or increased need to clear your throat
- Itchy eyes or mouth
- Sneezing
- Aches and pains: muscle, joint, tendon, or ligament
- Changes in skin: rashes, acne, dry skin, little pink bumps or spots, dry hair or nails
- Mood issues: mood swings, feeling low or depressed
- Feeling anxious, less able to handle stress
Suggested Order of Reintroductions
When it comes to food reintroductions, there is no right or wrong way to choose where to start. A very good argument can be made that the first foods you reintroduce should be the ones you miss the most. Another argument can be made for reintroducing first the foods that are least likely to cause a reaction or that have the most redeeming qualities.
The following suggested order of food reintroductions takes into consideration both the likelihood of reaction (based on what science says about how that particular food interacts with the gut barrier or the immune system) and the inherent nutritional value of the food. There are four stages. The first stage includes foods that are most likely to be well tolerated or are the most nutrient dense. The second stage includes foods that are less likely to be well tolerated or are less nutrient dense. The third stage includes foods that are even more unlikely to be well tolerated, but still have compelling nutrition. The fourth stage includes foods that are most likely to be untolerated and that you may wish to never challenge.
Challenge all the foods in stage 1 that you want to reincorporate (except any that you are allergic to or have a history of severe reactions to) before moving to stage 2. Follow the same protocol before moving from stage 2 to stage 3 and then from stage 3 to stage 4. You don’t have to tolerate all the foods in stage 1 to be able to move to stage 2, but if you don’t tolerate many (or most) of the foods, take a break from new food reintroductions for a few weeks or even months and then rechallenge those stage 1 foods. If you still react to them, wait a few more weeks and then start challenging stage 2 foods (keeping the untolerated ones from stage 1 out of your diet).
STAGE 1 FOODS
- egg yolks
- fruit-, berry- and seed-based spices
- seed and nut oils
- ghee (from grass-fed dairy)
- occasional coffee
- cocoa or chocolate
- peas and legumes with edible pods (green beans, scarlet runner beans, sugar snap peas, snow peas, etc.)
- legume sprouts
STAGE 2 FOODS
- seeds
- nuts
- chia seeds
- coffee on a daily basis
- egg whites
- grass-fed butter
- alcohol in small quantities
STAGE 3 FOODS
- eggplant
- sweet peppers
- paprika
- peeled potatoes
- grass-fed dairy
- lentils, split peas, and garbanzo beans (aka chickpeas)
STAGE 4 FOODS
- chili peppers and nightshade spices
- tomatoes
- unpeeled potatoes
- alcohol in larger quantities
- gluten-free grains and pseudograins
- traditionally prepared or fermented legumes
- white rice
- foods you are allergic or have a history of strong reactions to
 Don’t Be Afraid!
Don’t Be Afraid!
It’s a surprisingly common experience to feel so good on the AIP that a person is afraid to try any reintroductions. But reintroducing eliminated foods is a critical step of your health journey. This is because some eliminated foods (like eggs, nuts, seeds, cocoa, coffee, and grass-fed A2 dairy) have some impressive nutritive value and can improve the overall nutrient density of your diet if well tolerated. Plus, the more dietary flexibility you have, the easier life is—you’ll have less difficulty traveling or eating in restaurants or at potlucks, work meetings, or any social situation.
The knowledge you glean from reintroductions is empowering. If a reintroduction goes well, you’ve got a new food to add to your diet, increasing the variety of foods you eat. If a reintroduction doesn’t go well, this is still great information! You now better understand the dietary triggers of your disease and which lines you can’t cross. And in the uncommon case where a reintroduction goes very poorly (the fear of which is what stops many people from even trying), remember that the AIP is an entire toolkit for healing. You have the knowledge and skills to recover quickly and get back on your feet. Just go back to 100% AIP, get plenty of sleep and low-strain activity, and stay hydrated until you feel better.
I also want to remind you that truly understanding the ins and outs of the AIP can help guide reintroductions and troubleshooting. I truly believe that knowledge is power. As a reminder, you can get there via self-education (reading my books and/or the vast collection of articles on the AIP on my site, for example), 1-on-1 coaching (like working with an AIP Certified Coach), group coaching (like SAD to AIP in Six), or a virtual classroom (like the AIP Lecture Series).
The post The Reintroduction Phase of the AIP appeared first on The Paleo Mom.